Journal of Indian Association of Pediatric Surgeons, Vol. 12, No. 2, April-June, 2007, pp. 85-88
Case Report
Biliary ascariasis
Sivakumar K, Varkey Sam, George MathanP, Rajendran S, Hema R
Department of Pediatric Surgery, SAT Hospital, Medical College, Trivandrum, Kerala
Correspondence Address:"Anusham" GRA-48, Main Road, Gowrisapattom, Trivandrum, Kerala - 695 004 kskdranusham@yahoo.co.in
Code Number: ip07031
Abstract
Ascaris lumbricoides, or the common roundworms, has a worldwide distribution but is mainly seen in Asian and Latin American countries. In humans the usual habitat is in the small intestine, mainly in the jejunum. But if the worm load is high, which may go up to a thousand worms, the worms tend to migrate away from the usual site of habitat. This brief paper aims at highlighting the condition of biliary ascariasis through the authors' experience in managing three such cases over a period of 1 year. The clinical features which arouse suspicion of biliary ascariasis, as well as diagnostic modalities and management, are described. Initially the cases were managed conservatively, but we conclude that if worms are retained in biliary tree for more than 10 days, surgery should be performed; since retention of degraded and calcified dead worm can occur, and this can lead to complications which are difficult to manage.Keywords: Ascaris lumbricoides, biliary tract, piperazine citrate, roundworms, ultrasonography
Introduction
Ascaris lumbricoides is endemic in costal areas of Kerala due to lack of basic sanitation. Four costal areas with a large slum population come under the coverage of our hospital. Though the number of admissions due to complications of adult roundworm infestation came down in recent years, we still manage 150 children with complications of roundworm infestation per year; most of these cases can be successfully treated conservatively. Biliary complications of roundworm infestation are very rare, constituting less than 2% of the total number of cases. In this report, we share our experience of managing three cases of biliary ascariasis; the symptomatology, diagnosis and management of biliary ascariasis are highlighted and the literature reviewed.Case Reports
Case 1
A 6-year-old boy was admitted with acute onset of severe abdominal pain which was not associated with fever, vomiting or urinary symptoms. The pain was almost constant and was relieved only with narcotics. His abdomen was soft and nontender. He was observed for 2 days. There was no relief of symptoms; hence an ultrasonography of abdomen was done, which revealed a dilated CBD with a roundworm inside - 'stripe sign'of roundworm [Figure - 1]A. The patient's liver function test and S/amylase values were normal. He was treated with antibiotics, antispasmodics and intravenous fluids. He was totally relieved of symptoms by the fifth day, and he was started on oral fluids. Piperazine citrate 75 mg/kg/day was given orally for 2 days. The patient passed several roundworms in motion. Repeat ultrasonography revealed that the worm was still inside CBD. He was given a dose of Albendazole and sent home. An ultrasonography after another 2 weeks revealed that the roundworm was still inside CBD. We planned to wait for another 2 weeks; and by the end of fifth week as the roundworm was still inside, laparotomy and CBD exploration were done. The necrotic and calcified materials inside CBD were washed out and CBD closed over a T-tube.
Case 2
A 9-year-old girl belonging to low socioeconomic group was admitted with acute onset abdominal pain of 5 days' duration, without any other associated symptoms. Her abdomen was soft and nontender. However, a routine ultrasonography revealed a dilated CBD with a roundworm inside, and one end of the roundworm was seen going into the gall bladder - 'inner tube sign'of roundworm [Figure - 1]B. Her liver function test and S/amylase were normal. She was treated conservatively and got relieved of symptoms in 2 days. Two doses of piperazine citrate and, later, albendazole were given. A repeat ultrasonography at the end of first week revealed the roundworm to be still inside the biliary tract. On the 10 th day, she underwent laparotomy and CBD was explored. A 25 cm long dead roundworm was removed from CBD.
Case 3
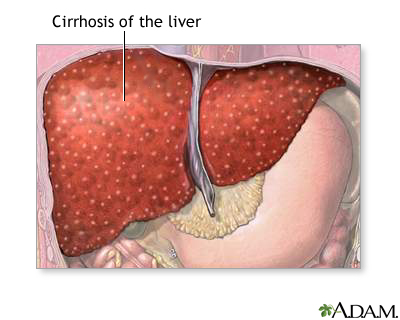
A 6-year-old girl was admitted with acute onset abdominal pain of 3 days' duration. There were neither any associated symptoms nor any specific physical findings. Ultrasound examination revealed dilated CBD with multiple linear shadows suggestive of multiple worms - 'spaghetti sign'of roundworm [Figure - 1]C. In the liver, there were hyperechoic shadows suggestive of pneumobilia [Figure - 1]D. In spite of multiple worms inside, she also became symptom free in 4 days. However, explored since worms still remained inside at the end of first week; and to our astonishment, there were 39 worms - dead and live - in CBD.
Results
All three patients recovered well after surgery. On follow-up ultrasonography after 2 weeks, they were found to have normal CBD and there was no evidence of any congenital biliary tract anomaly.
The first patient was readmitted with features of cholangitis, 11 months after the initial laparotomy, and an ultrasonography revealed dilated CBD with a calculus inside. He is waiting for surgery.
Discussion
The normal habitat of roundworms is the jejunum, but they can migrate to the biliary tract through sphincter of Oodi. Ironically, in the life cycle of Ascaris the larvae reach the liver through the portal vein and live there for 3-4 days before going to the lung. [1]
The most common presenting symptom of biliary ascariasis is pain, which is more constant than colic. Rarely it can produce pancreatitis, cholangitis, liver abscess and even perforation of CBD or gall bladder. [2] In our hospital, we did not come across such complications proven to be due to Ascaris. There are reports of these complications from Jammu and Kashmir, where biliary complications constitute 11% of total admissions for complications due to roundworm infestation. [2]
Ultrasonography is the investigation of choice for diagnosis and follow-up. There are specific sonographic features described for ascariasis in CBD: 'inner tube sign'- roundworm seen as a thick echogenic stripe with a central anechoic strip, which is the intestinal tract of worm; 'stripe sign'- roundworm seen as a non-shadowing stripe without inner tube; and 'spaghetti sign'- overlapping longitudinal interfaces in the CBD due to coiled single worm or due to multiple worms. [3] In this series, the first author did ultrasonography.
Our experience with the first case was that a waiting period of 5 weeks resulted in degraded worms, which were difficult to clear from CBD. Therefore, in the other two cases, we decided to operate earlier though the patients were asymptomatic; and the results were good. This is in contrast to a large series reported from Jammu and Kashmir where only 11% of patients with biliary ascariasis needed surgery. [2] The long-term follow-up results of these cases were not available. We feel that a waiting period longer than 10-15 days is not advisable due to the fact that once roundworm is dead, its protective outer cuticle (a hyaline noncellular layer, forming integument of nematodes) [1] will disintegrate and bile easily digests the worm.
ERCP can help to diagnose and extract biliary and pancreatic ascariasis, where sphincterotomy and Dormia basket can be used. [4],[5],[6] We don't have ERCP facility; hence it was not attempted. If facilities for endoscopic treatment are available, it should be the choice in the current era.
The incidence of biliary ascariasis after surgery on biliary tract, like sphincterotomy or Roux-en-Y hepaticojejunostomy, is expected and such cases have been reported. [6],[7]
The conservative treatment is by keeping the patient nil by mouth, antispasmodics, antibiotics and intravenous fluids. Once the pain gets relieved, it means either the worms have escaped from biliary tree or they are dead. Dead worms, if they remain there, can produce late complications like recurrent cholangitis and can act as a nidus for calculi formation. In one series, intrahepatic duct and bile duct calculi developed in 7 out of 500 adult patients studied, in whom dead worms formed the nidus of stone. [8] In another series, 4 out of 109 adult patients with biliary ascariasis were operated as the worms were trapped in the ducts, which led to stone formation with worm fragment as nidus. [9] There are pathological reports of roundworm forming nidus for stone formation. [10] Hence we recommend early exploration and removal.
Oral antihelminthic piperazine citrate is given to expel the worms from intestine before surgery. We prefer piperazine citrate since this produces flaccid paralysis of worms; unlike mebendazole or albendazole, which produce spasticity of worms. Flaccid paralysis is important since roundworms tend to remain in the bowel by its muscle tone. [1] We always give albendazole few days after piperazine citrate, since piperazine is useful only for adult roundworms. Albendazole is a broad-spectrum antihelminthic, larvicidal and ovicidal. Immobilization and death of susceptible gastrointestinal parasite occur slowly with albendazole, and their clearance from intestine may not be complete until a few days after treatment. [11] There is no literature statement that piperazine citrate is superior to albendazole, but its mechanism of action is important in cases of roundworm overload, especially in situations where roundworm forms masses inside intestine. Piperazine citrate is recommended for gastrointestinal and biliary obstruction secondary to ascariasis. [12]
Conclusion
In all patients with constant severe pain in the abdomen without any specific physical findings reporting from endemic areas for Ascaris, ultrasonography should be done to rule out biliary ascariasis. The main differential diagnoses are early pancreatitis, ischemic enteritis (rare, nowadays in Kerala) and malingering. Ultrasonography is the investigation of choice for diagnosis and follow-up. If the worm/worms tend to remain in biliary tree even after 10 days, it/they should be removed surgically or endoscopically even though the child is symptom free.References
| 1. | Chatterjee KD. Ascaris lumbricoides Linnaeus, 1758. In : Chatterjee KD. Parasitology, 12 th ed. Chatterjee Medical Publications: 1981. p. 160-88. Back to cited text no. 1 |
| 2. | Wani MY, Ahmed Bashir, Wani AN, Pandita S. Our experience with biliary ascariasis in children. J Indian Assoc Pediatr Surg 2005;10:S8. Back to cited text no. 2 |
| 3. | Rama A, Mahinder KN, Gupta A, Kamal VI. Images: Biliary ascariasis. Indian J Radiol Imag 1999;9:1:23 Back to cited text no. 3 |
| 4. | Parente F, Bargiggia S, Anderloni A, Bianchi Porro G. An unusual cause of recurrent biliary colic. Dig Liver Dis 2004;36:763-5. Back to cited text no. 4 |
| 5. | Misra SP, Dwivedi M. Clinical features and management of biliary ascariasis in non-endemic area. Postgrad Med J 2000;76:29-32. Back to cited text no. 5 |
| 6. | Sandouk F, Haffar S, Zada MM, Graham DY, Anand BS. Pancreatic-biliary ascariasis experience of 300 cases. Am J Gastroenterol 1997;92:2264-7. Back to cited text no. 6 |
| 7. | Braga LH, Tatsuo ES, Guimarγes JT, Miranda ME, Paixγo RM, Teixeira CR, et al . Biliary ascariasis after Roux-en-Y hepaticojejunostomy. J Pediatr Surg 2000;35:1394-5. Back to cited text no. 7 |
| 8. | Khuroo MS, Zargar SA, Mahajan R. Hepatobiliary and Pancreatic ascariasis in India. Lancet 1990;335:1503-6. Back to cited text no. 8 |
| 9. | Khuroo MS, Zargar SA. Biliary ascariasis. A common cause of biliary and pancreatic disease in an endemic area. Gastroenterology 1985;88:418-23. Back to cited text no. 9 |
| 10. | Pilankar KS, Amarapurkar AD, Joshi RM, Shetty TS, Khithani AS, Chemburkar VV. Hepatolithiasis with Biliary ascariasis: A case report. BMC Gastroenterol 2003;3:35. Back to cited text no. 10 |
| 11. | James WT, Leslie TW Jr. Antihelminthic drugs. In : Godman and Gilman's. The Pharmacological basis of Therapeutics. 9 th ed. McGraw Hill Companies Inc: 1987. p. 1010-20. Back to cited text no. 11 |
| 12. | Michael EG, Ascariasis. E-medicine. [Last updated on 2005 Mar 23]. Available from: http://www.emedicine.com/ped/ |
Copyright 2007 - Journal of Indian Association of Pediatric Surgeons