--------------------------------------------------------------------------------
Understanding Biofilm and Lyme Disease
by Dr. Bill Rawls | August 27, 2015
Biofilms are colonies of microbes. They chiefly contain bacteria, but biofilms can also include protozoa and fungi. Biofilms can form anywhere there is moisture and a surface. In other words, everywhere—including many surfaces inside the human body.
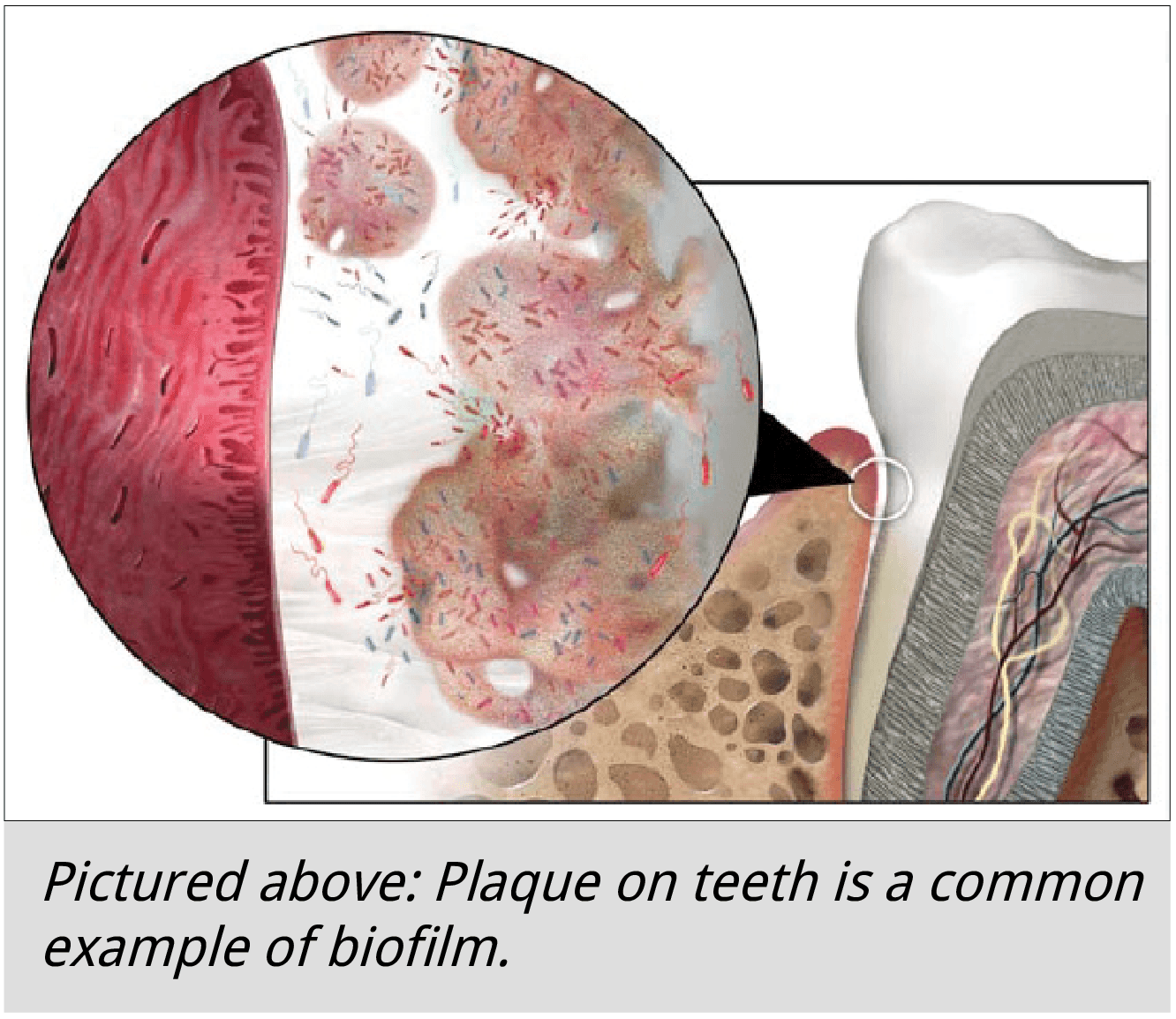
The ring inside your toilet bowl and plaque on your teeth are examples of biofilm.
Biofilms are initiated by certain types of bacteria that are able to attach to a moist surface with special adhesion structures called pili. Once adhesed to the surface, bacteria stick together and start producing a matrix of slime (called extracellular polymeric substance, or EPS).
Once the matrix is established, other kinds of microbes can join in. Imagine a crowded dance floor with bodies squeezed together forming a uniform mass, swaying to the rhythm of the music. That’s the feel of a biofilm.
A polysaccharide shell on the surface of the biofilms protects the organisms inside from starvation, drying out, the immune system, and antibiotics. The surface can include minerals, such as calcium, and blood products including fibrin.
Safe inside the biofilm, microbes are free to mingle and exchange information. Communication between microbes, called quorum sensing, is accomplished by signaling molecules. Once a community is formed, certain groups of microbes take on specialized roles of performing metabolic functions for the entire unit. Water channels develop within the biofilm for moving nutrients and signaling molecules. The biofilm grows by cell division and recruitment of new individuals.
In essence, the biofilm becomes an organism in itself.
Biofilms are as ancient as any lifeform. They were likely the bridge between single cell organisms and higher multi-cell organisms.
Biofilms cause illness by damaging the surfaces to which they attach to. If a biofilm becomes massive enough, it can cause obstruction.
Once a biofilm reaches a certain size, it disperses, allowing inhabitants to spread and colonize other surfaces. Spreading biofilms accelerate damage. Bacteria in the body are constantly trying to form new biofilms and the immune system is constantly breaking them down.
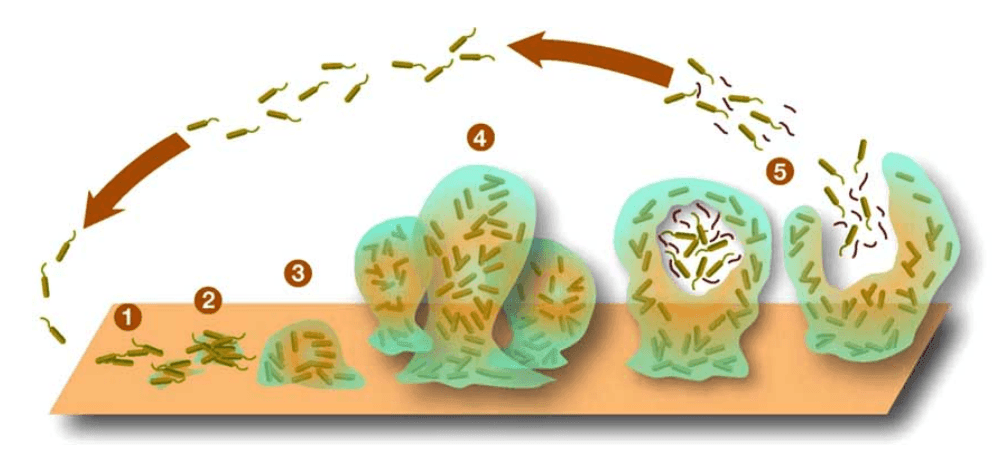
Above: The five stages of biofilm development are (1) initial attachment, (2) irreversible attachment, (3) maturation I, (4) maturation II, and (5) dispersion.
Typical biofilm diseases occur where there are surfaces for the biofilm to form. Examples of biofilm diseases include:
Biofilms readily occur in the intestinal tract. In fact, formation of biofilms in the colon and appendix are quite normal and are supported by the immune system. It may be a mechanism for reinoculating the gut with favorable bacteria.
Lately, there is a lot of talk on Lyme forums about Lyme disease being a biofilm disease. It seems to stem from a study done in a lab showing that borrelia, the bacteria associated with Lyme disease, can form biofilm.
It is well known that borrelia can form biofilm inside a test tube. Forming and participating in biofilm is a natural trait for most bacteria. In fact, if you can’t form a biofilm, you’re not much of a bacteria.
The symptoms associated with Lyme disease, however, are not typical of biofilm diseases. Symptoms of Lyme disease are caused by the bacteria manipulating the immune system to generate inflammation. Inflammation breaks down tissues and allows the bacteria to access vital nutrients.
When it comes to biofilms in the body, it wouldn’t be surprising to find that borrelia is able to join the party, but once inside the biofilm it would lose its ability to manipulate the immune system, and therefore lose its ability to cause symptoms. That said, biofilms are not how borrelia causes illness.
Immune dysfunction caused by borrelia, however, could allow biofilms in the body to flourish. This may be a factor in intestinal disease that usually accompanies Lyme disease and skin diseases sometimes associated with Lyme disease (but it is probably a very small factor compared to other things). Calcium deposits in the inner ear causing dizziness may also be associated with biofilm.
As to whether biofilms prevent antibiotics from eliminating borrelia, there are other factors that actually play a greater role in determining antibiotic resistance. Borrelia grows very slowly, exists in low concentrations in the body, is able to bore deeply into cartilage and brain tissue, and can live inside cells—all factors that enhance resistance to antibiotic therapy.
Though Lyme disease is not a biofilm disease, it is a good idea to support the body’s ability to deal with biofilms during any illness.
A healthy immune system is the best way to slow formation of biofilm in the body. The immune system is constantly breaking down new biofilms that start to form—it’s part of the everyday struggle of life.
Any herbal therapies or essential oils with antimicrobial and immune enhancing properties are beneficial for controlling biofilm.
Digestive enzymes help with digestion, but also help break down biofilm in the gut. Systemically absorbed enzymes may also help dissolve other biofilms in the body.
N-acetyl cysteine (NAC) is known to break up mucous and may also play a role in dissolving biofilm.
EDTA, a chelating agent, removes minerals from the biofilm surface and can help break up a biofilm (but can also remove essential minerals from the body at large).
Oxygen and nitric oxide penetrating into the biofilm can help degrade the biofilm.
Blasting biofilms with strong chemicals and potent antibiotics doesn’t work because it suppresses immune function. Supporting healthy immune function and etching away until the biofilms are gone is the best approach.
1. Supi et al, Characterization of Biofilm Formation by Borrelia burgdorferi, In Vitro, PLOS-one, Oct 24, 2012
2. Karatan E, Watnick P, Signals, Regulatory Networks, and Materials That Build and Break Bacterial Biofilms, Microbiology and Molecular Biology Reviews, June 2009, Vol 73 (2), P. 310-347
3. Lennox J, Biofilm Development, Biofilms: The Hypertextbook, Web, May 2011
4. Costerton, Stewart, Greenburg, Bacterial Biofilms: A Common Cause of Persistent Infections, Science, May 1999, Vol 284 (5418) p. 1318-1322
5. Sapi, MacDonald, Biofilms of Borrelia burgdorferi in chronic cutaneous borreliosis, Am J Clin Pathol, 2008, 129, p. 988-989
6. Hoyle, Costerton, Bacterial resistance to antibiotics: the role of biofilms, Prog Drug Res, 1991, 37, p. 91-105
7. Kurti, Munderloh, Ashstrand, Colony formation and morphology in Borrelia burgdorferi, J Clin Microbiol, 1987, 25, p. 2054-2058
8. Figure copyright 2006 Keith Kasnot, MA, CMI, FAMI
9. codicepaleo.com/wp-content/uploads/2014/07/Biofilm-formation.png
10. Image source: http://nutritionreview.org/2014/08/gingivitis-gum-health/